WELCOME TO THE PROVIDER PULSEDecember 2025 INDEX:
|
|
|
|
VACCINE PREVENTABLE DISEASERESPIRATORY VACCINE ORDERING AND MANAGEMENTDue to the excessive dollar amount of respiratory vaccine wasted in 2024, more than $1,000,000 in COVID wastage alone, DOH has had to implement stricter guidelines in vaccine ordering and allocation. CVP and AVP enrolled provider sites are required to order no more than vaccine usage for the same month of the previous year at a time. Orders for respiratory products; RSV, COVID and Flu; are allowed on a weekly basis based on current inventory and anticipated need. This allows sites to better monitor inventory. Provider sites are encouraged to store the vaccine appropriately, for example, Moderna vaccines should be kept in the freezer and thawed based on the clinics need for that day. Much of the wasted was from sites who stored Moderna in the refrigeration, and it was past the 60 day beyond use date for refrigeration storage. Beyond use dates are required on all refrigerated boxes of Moderna. Appropriate vaccine management and inventory control will allow the program to continue. Thank you for doing your part. |
|
|
|
Flu Season Alert and Local Flu Death ReportInfluenza (flu) is a highly contagious disease caused by influenza viruses and symptoms include fever, headache, cough, and sore throat. The flu may be caught at any time of the year but is more common during the colder months. It is usually spread from respiratory droplets from an infected person’s cough or sneeze that may be inhaled by others in proximity. In order to prevent the flu, we highly encourage everyone ages 6 months and up to receive their annual flu vaccine from September to October. Vaccination should continue throughout the season for as long as Influenza viruses are circulating. Certain populations may be at greater risk of getting the flu, including those 65 years and older, those with weakened immune systems, individuals with certain disabilities such as decreased muscle or lung function, pregnant women, and those living in nursing homes and long-term care facilities. To learn more about those that are at risk, please refer to the web page linked here. By protecting yourself, you also help protect others by not spreading illness. Getting the flu vaccine lowers the chances of becoming ill and reduces the severity of illness, which can be the difference between recovering at home and ending up in the emergency department. With the holidays coming up, it’s important to stay up to date with your flu vaccine or avoid gathering anyone is when sick. It’s a good idea to get vaccinated at least two weeks before a family gathering or your planned departure date. This gives your body enough time to build up immunity and offer protection. If you get the flu, please stay home if you are ill. Wear a mask over your nose and mouth in indoor public spaces when flu or other respiratory viruses are circulating at high rates, cover coughs and sneezes, and wash your hands thoroughly with soap and water and use hand sanitizer when soap and water isn't available. Snohomish County residents can visit local pharmacies and clinics to get vaccinated. In Washington state, children under age 19 can be vaccinated at no cost while most insurance plans, including Medicare part B, cover the cost for adults. If a person still needs a COVID-19 vaccine, both vaccines can be given during the same visit. For the most up-to-date information on influenza activity for Snohomish County, you may review the influenza dashboard. For more information about the flu, please visit the Washington State DOH Flu facts page or contact the Snohomish County Health Department Immunization and Vaccine Preventable Disease Team at 425-339-5234. To read more about the first flu death in Snohomish for 2025-2026 Season (released 11/12/25): Snohomish County Reports First Flu Death of 2025-2026 Season • Snohomish County Health Department, WA
|
|
|
|
healthy communitiesSTATE MANDATORY SUICIDE PREVENTION TRAININGIs it time to obtain or update your CEUs with the State mandatory suicide prevention training? Legislation (RCW 43.70.442) requires that health professions, including school nurses and mental health professionals, take a suicide prevention course that meets their hour and content requirement before the end of the next full continuing education reporting period. Implementation dates vary by profession. For specific questions about your own suicide training requirements or whether a particular training is appropriate for your health profession, please contact the program manager or executive director of your profession's board or commission. Please visit the WA State DOH for all you need to know about this requirement including a list of trainings found here https://doh.wa.gov/public-health-provider-resources/healthcare-professions-and-facilities/suicide-prevention/training-requirements. |
|
|
|
CHILD FATALITY REVIEW DATA AND RECOMMENDATIONS IN SNOHOMISH COUNTYChildren are the future of our community. We all play a role in keeping them safe and helping them to thrive. The untimely loss of any child’s life is a tragedy for the child’s family and our community – especially when the loss is preventable. Understandably, when a community is affected by a child’s death, it wants answers about how and why the child died. These answers can help communities have a clearer understanding of underlying risk factors and inequities that they may not identify otherwise.
To better understand how we can prevent child fatalities, the Snohomish County Health Department uses a process known as Child Fatality Review (CFR) to examine the circumstances so we can identify risk factors and prevention interventions. The information collected through the review process informs recommendations for data-driven prevention strategies. Data tells the story and helps us determine action and priority. To learn about child fatality data and recommendations in Snohomish County, visit https://www.snohd.org/1821/Child-fatality-review-and-prevention. If you have any questions about CFR, contact Wendy Burchill at wendy.burchill@co.snohomish.wa.us.
|
|
|
|
SUBSTANCE USE PREVENTIONNEW ICD-10-CM CODE FOR CANNABINOID HYPEREMESIS SYNDROMEA new ICD-10-CM diagnosis code for Cannabinoid Hyperemesis Syndrome (CHS) went into effect on October 1, 2025. ICD-10-CM codes are used to classify different medical diagnoses, symptoms, and procedures in health records and for billing and claims processing. To date, most health systems have documented CHS using a combination of codes for nausea and vomiting, such as R11.2, and a second code indicating cannabis use or cannabis use disorder. With the new code, a direct diagnosis for patients with CHS can be recorded, which will help with monitoring and treatment of the condition, as well as make it easier for researchers to collect data for public health research on cannabis-related health issues. CHS is an increasingly recognized complication of frequent and long-term cannabis use, characterized by intense abdominal pain and recurrent episodes of nausea and intense vomiting. Symptoms typically begin abruptly within 24 hours of the last cannabis use. Two studies (see below) published in 2025 have revealed a sharp rise in CHS-related emergency department visits in the U.S.: - The first reported a 49% annual increase among individuals aged 13–21 between 2016 and 2023.
- The second found a 28.1% annual increase among those aged 15–24 from 2006 to 2020.
The addition of this diagnosis code demonstrates a growing awareness of the unique health conditions linked to cannabis use and can help lead to more support for public health policies and programs related to cannabis use. This notice was written in collaboration between ADAI and the Snohomish County Health Department. - Toce MS, Monuteaux MC, Fishman MD, Hudgins JD. Emergency Department Visits for Cannabis Hyperemesis Syndrome Among Adolescents. JAMA Netw Open. 2025;8(7):e2520492. doi:10.1001/jamanetworkopen.2025.2049
- Jack B, Susi A, Reeves P, Nylund CM. Increasing trends of cannabinoid hyperemesis syndrome in youth: The grass is not always greener. J Pediatr Gastroenterol Nutr. 2025;80(4):638-643. doi:10.1002/jpn3.12469
|
|
|
|
TUBERculosisTB Routine Testing ReminderAre you testing patients born outside the U.S. for TB? National data shows half of healthcare providers are considering TB for non-U.S.-born patients. Identifying and overcoming barriers to TB testing and treatment is crucial. Anyone born outside the U.S. or Western Europe should be tested for TB at least once. For positive results, contact the health department for guidance at 425.339.5225. Let's work together to reduce TB transmission in Snohomish County. Key Points to Remember: Think TB if patients have symptoms like a persistent cough, fever, unexplained weight loss, night sweats, or related radiological findings. High-Risk Groups Include: - Close contacts of active TB cases
- Those with a history of residence or travel to TB-endemic regions (refer to the WHO table)
- Children under 5 with a positive TB test
- Individuals with a history of latent TB infection (LTBI), especially if diagnosed in the past 2 years
- Residents or workers in shelters, correctional, or long-term care facilities
- People with HIV, diabetes, or other immunocompromising conditions
TB-Endemic Regions (2019 Data from WHO list of high burden countries): - Severely Endemic (500+ cases/100,000): Central African Republic, Gabon, Lesotho, South Africa; DPR Korea; Philippines.
- Highly Endemic (300-499 cases/100,000): Angola, Congo, Democratic Republic of Congo, Eswatini, Guinea-Bissau, Liberia, Mozambique, Namibia, Zambia; Indonesia, Myanmar, Timor-Leste; Kiribati, Marshall Islands, Mongolia, Papua New Guinea.
- Endemic (100-299 cases/100,000): Various regions in Africa, the Americas, Eastern Mediterranean, Europe, South-East Asia, Western Pacific.
|
|
|
|
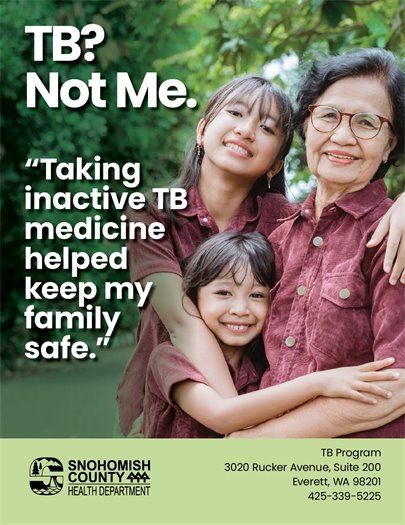 New printable flyers available here RESOURCES: |
|
|
|
|
|